Superior border of the arcuate line: Three dimension reconstruction and digital measurements of the fixation route for pelvic and acetabular fractures
2015-02-04 文章来源:上海交通大学附属上海市第一人民医院 我要说
Author:Ji Xiaoxi & Wang Fang & Wang Dongmei & Li Fan &Li Xiaoqin & Su Yunlong & Zhang Jie & Wang Qiugen
Introduction
Comparedto along bone, the shape of the pelvis is morecomplex and irregular. Thus, plate shaping of the pelvis during surgeryis not perfect. In fact, repeatedly shaping the reconstructionplate during the operation is more likely toresult in prolonged operation time, breakage of the inter-nal fixator, and loss of stage I reduction due to the mismatch of the shape of implantandpelvis. All of the problems mentioned above increase the risk of the operation and theincidence of complications . For rotationally unstablepelvic fractures and peri-anterior column fractures of the acetabulum (including fractures of the anterior wall, anterior column, transverse fractures,T-shaped fractures, and frac- tures of the anterior columnor anterior wall associated with a hemi-transverse fracture), the incidence is relativelyhigh (52.4 % and 47.5 %, respectively) . The effects of thereduction and fixation of the fractures directly determine the occurrence of postoperative complications and the patient’s quality of life . The two groups of fractures usuallyresult in ruptures of the pelvic anterior ring, especially of the arcuate line. Therefore, to fix the aforementioned fractures,the inferior border of the iliac fossa and its forwardexten- sion are commonly chosenas areas to place the reconstruc- tionplate . This region is considered an ideal implant location, because it provides clear surgical exposure, aflatbone surface, and relativelythick bone tissue. According to the specificfracture type, the reconstruc- tion plate can extend along the pubic tubercle,pubis pecten, iliopubic eminence, arcuate line, or it may ap- proach the sacroiliacjoint. Letournel et al. reported that fixing the anterior wall, anterior column, or a fracture that extended outof thehip joint, couldbe accom- plished by positioning a long reconstruction plate along the pubis pectento thearcuateline .Jakob et al. treatedanterior column fractures of the acetabulum and pelvic ring fracturesby placing the plate along the superior ramus ofthepubis or the iliopubic eminence to the arcuate line. By doing this, the authors achieved satisfactory anatomic reduction . At present, due to thecomplex and irregular shape of the pelvis compared to a long bone, and the multi-plane and multi-radian fixation route in3D, no anatomical data for the fixation route along the supe- rior border of the arcuate line is currentlyavailable,whichresults in an inefficient and ineffective plate shaping proce- dure. Digital three-dimensional (3D) measurements, based onCT reconstruction, have the same accuracy and reliability astraditional measurements, and this 3D technology has beenconsidered a more efficient method for orthopaedic anatomic studies, design, and optimization ofimplants. Thus, the first hypothesiswasraised to obtain an optimized plateshape of pelvic fixator by digital 3D anatomical measure- ments, which eliminates the prolonged operation time, break-ageof the fixator and loss of stage I reduction.
Unlike other humanbones, the pelvic shape appears markedly different between males and females. For the female pelvis alone, there are four differentshapes, which are termed gynecoid, android, platypelloid and anthropoid. Although finding a perfect match for each pelvic shape can offer the maximalanatomical matches between the internal fixator and the pelvis, it is relatively unrealisticand costly for industrial manufac-ture.Differences among pelvic shapes are related to thechanges of thepelvic inlet shape; in particular, tothe ratio of the posteriorsagittal diameter to the anteriorsagittal diameter (DSp/DSa) andtheratioof thetrans- verse diameter to thesagittaldiameter (DT/DS). With the increaseof DSp/DSa and DT/DS, the pelvic inletshape transitions fromthe heart-shapeof the android type to the approximately round, elliptical shape of thegynecoid and platypelloid types . Hence, the second hypothesis was raised to find the relationship betweenDSp/DSa, DT/DS and the shape of the superior border of the arcuate line, which could used as a base on which to estimate the general shape of the internal fixator by pelvic type.
A retrospective observational study by digital recon- structionand 3D measurements of a large sample of normal adult pelvic CT scans was conducted by the authors. Theaimof thisstudy wasto obtaina series of parameters describing theshape andbone thicknessof the fixation route along the superiorborder of thearcuate line to the pubic tubercle, and find the relation between DSp/DSa, DT/DS and the shape of the superior borderof the arcuate line; and finally, to provide a good reference for pelvic and acetabular surgeries and the design of pelvic anatomical internal fixators at the su- perior border of the arcuate line.
Patients and methods
Samples and equipment
We collected the computed tomography scans from out- patients with varicoseveins of the lower limb, who needed enhanced computed tomography scan (CT scan) from pelvis to feet. Each patientwith pelvic deformity,trauma, tumor and other diseases on CT scans and intheir history was eliminated.From December 2009 to November2010,175 complete pelvic computed tomography scans of unrelated ethnic HanChinese adults (meas age 61.0years;105 men,70 women) were collectedfrom the medical image database of the department of radiology of a largecomprehensive hospital.The age distribution of all 175 patients is seen in Table 1. During CT scanning, patients kept the standard anatomical horizontal position with lower limbs unbent. All the CT scanswere performedat 12 kV and 300 mA with a slice thickness of.75mmby a 64- channelCT, Light Speed VCT XTe (GE Healthcare; Milwaukee, WI, USA), and the scanning time of each slice was 20ms. There were approximately380DICOMformat CT images for the pelvic part of eachpatient. For the data that was collected from outpatients,the height and weight of the patient were not recorded inthis study. The study was performed with the help of the following software: the interactivemedical image control system MIMICS 13., the reverseengineering software Geomagics 10, and the mechanical design soft-ware Unigraphics NX. The study was approved by the Review Board of Shanghai First People’s Hospital.
Table1 Age distribution of all 175patients
21–30 yrs | 31–40 yrs | 41–50 yrs | 51–60 yrs | 61–70 yrs | 71–80 yrs | ≥ 81 yrs | |
Male | 4 | 5 | 5 | 16 | 17 | 9 | 5 |
Female | 2 | 11 | 13 | 30 | 24 | 21 | 13 |
Total | 6 | 16 | 18 | 46 | 41 | 30 | 18 |
Measurement of parameters
Each volunteer’s DICOM format CT images were imported to Mimics 13.. After removing the soft tissue by thresholding segmentation, region growing, and a subsequent smoothing process, an entire 3D digital pelvic model was established andsaved in Stereo Lithography (STL) format.
The pelvic model was importedto the Geomagics soft- ware as a mesh model in the STL format. The horizontal, coronal and sagittal plane were determined in the first place.According to the standard anatomical position, the pubictubercle and anterior superior iliac spineare in the same coronal plane. The plane passing the midpointof the pubic symphysis, the midpoint of the anterior border of the sacral promontory and the coccyxtip was identified the sagittal plane.The plane constructed perpendicularly to the sagittaland the coronal plane was the horizontal plane. Along with the route from the pubictubercle, pubis pecten, iliopubiceminence, arcuate line, and sacroiliac joint, several pointswere picked at the cortical surface, 10 mm lateralto the pelvic brim in the superior border of the arcuateline, to draw
the space curve of the bone surface. By intersecting extru- sion,the required measurement model and the anatomicalcurve were extracted.
The measurement model and the anatomical curve wereimported to UG in the STL and IGES format. Thus, the total length of the curve (L) can be measured. Bydividing the curve into elevenequal parts, the radius of curvature at eachdecile point, r1, r2, …, r1, and the bone thickness of eachdecile point, d1, d2, …, d10, were achieved from front toback. The curve section was divided into front-acetabular,acetabular, and post-acetabular areas by the locationof the acetabulum, and the thinnest bone regions of thethree parts, D1, D2, D3, were measured (Fig.1).
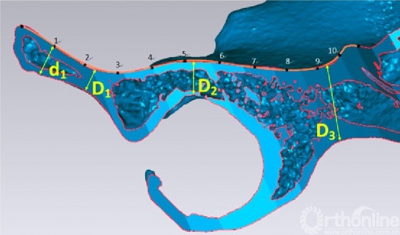
Fig.1 By dividing the curve into ten equal parts,theradius of curvature at each decile point,r1,r2,…,r10,and
the bone thickness of each decilepoint,d1,d2,…,d10,were achieved from front to back.The thinnest bone regionsof the three parts,D1,D2,D3,were measured
The pelvis wasimported to the Imageware 12.0 software as a mesh model in the STLformat. After being rotated to the position of the pelvic inlet, and compressingthe pelvis to the inlet plane as with X-ray films, the transverse diameter of thepelvic inlet DT(the widest distance), the sagittal diameter DS (the distancefrom the anterior border of the sacral promontory to the posterior border of thepubic symphysis), the anterior sagittal diameter DSa, and the posterior sagittal diameter DSp could all be measured (Fig.2). Finally, the ratio of the posterior sagittal diameter to the anterior sagittal diameter (DSp/DSa) and the ratio of the transverse diameter to the sagittal diameter (DT/DS)were calculated.
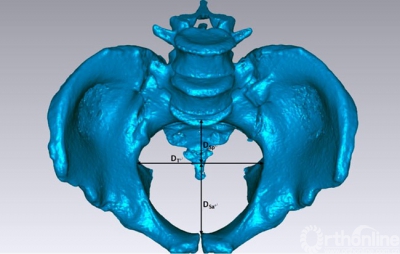
Fig.2 In the position ofthe pelvic inlet,just like the inletX-ray plane,the transverse diameter of pelvicinlet DT,the sagittal diameter DS,the anterior sagittal diameter DSa,and the posrerior sagittal diameter DSpwere measured
Statistical analysis
The data were expressed as mean ± standard deviation andanalyzed by using the descriptive methods with SPSS19.0. The data distributions were analyzed with normality tests.A p value less than 0.05 was considered to be statistically significant.
All the pelvis were categorized into seven groups by DSp/DSa (≤0. 40, 0.41–0.5, 0.51–0.6, 0.61–0.7, 0.71–.8, .81–.9, ≥ .9), and the relationship between theradius of curvature and the decile point was analyzed. Each group was tested and showed normal distributed. For eachgroup, we compared the mean values of the radius of curva-turebetween two adjacentpoints from decile point 1 to 10 with the T test.
Results
The radius and the bone thickness of curvature at each decilepoint are seen in Table 2 and Table 3. The thicknessof the front-acetabular, acetabular, and post-acetabular areas were 11.67± 2.94, 13.97 ± 3.36, and 28.21 ± 3.46 mm, respectively (Table 4). The transverse diameter, the sagittaldiameter, the anterior sagittal diameter, andthe posterior sagittal diameter of the pelvic inlet were 124.14 ± 11.69, 107.38 ± 13.51,66.01 ± 9.15, and 41.36 ± 8.19 mm, respectively (Table 5).
Table 2 The radius of curvatureat each decile point
| r1 | r2 | r3 | r4 | r5 | r6 | r7 | r8 | r9 | r10 |
Total (mm) | 29.18 ± 15.53 | 53.29 ± 16.26 | 43.04 ± 14.42 | 59.62 ± 21.02 | 93.67 ± 13.01 | 76.9 ± 18.66 | 75.76 ± 15.87 | 61.75 ± 16.68 | 54.62 ± 14.88 | 43.61 ± 19.10 |
Male (mm) | 24.51 ± 10.86 | 48.86 ± 20.84 | 35.96 ± 9.38 | 59.54 ± 22.92 | 87.2 ± 16.15 | 72.00 ± 16.91 | 77.07 ± 19.23 | 61.93 ± 18.31 | 51.68 ± 14.05 | 42.17 ± 19.64 |
Female (mm) | 36.10 ± 12.33 | 60.13 ± 17.30 | 53.55 ± 14.24 | 59.72 ± 18.07 | 92.57 ± 18.69 | 97.17 ± 18.37 | 73.84 ± 10.05 | 61.48 ± 14.01 | 59.01 ± 15.09 | 45.77 ± 18.20 |
P Value | 0.0002 | 0.0007 | 0.0001 | 0.955 | 0.467 | 0.001 | 0.423 | 0.860 | 0.001 | 0.226 |
Table 3 The bone thickness of each decile point
| d1 | d2 | d3 | d4 | d5 | d6 | d7 | d8 | d9 | d10 |
Total (mm) | 21.78 ± 9.48 | 14.14 ± 5.07 | 12.9 ± 2.96 | 23.53 ± 7.18 | 18.8 ± 7.61 | 15.55 ± 3.48 | 29.91 ± 14.78 | 46.03 ± 9.43 | 33.12 ± 6.15 | 30.41 ± 4.06 |
Male (mm) | 23.24 ± 9.78 | 14.93 ± 4.53 | 13.92 ± 2.75 | 25.93 ± 7.13 | 19.09 ± 5.16 | 17.09 ± 3.05 | 28.49 ± 13.75 | 49.38 ± 9.16 | 35.77 ± 6.05 | 31.28 ± 4.12 |
Female (mm) | 19.61 ± 8.63 | 12.97 ± 5.63 | 11.38 ± 2.62 | 19.95 ± 5.65 | 18.38 ± 10.26 | 13.27 ± 2.76 | 32.03 ± 16.06 | 41.07 ± 7.48 | 29.19 ± 3.75 | 29.13 ± 3.63 |
P Value | 0.013 | 0.012 | 0.0008 | 0.0006 | 0.547 | 0.0003 | 0.134 | 0.0003 | 0.0005 | 0.001 |
Table 5 The parameters of the pelvic inlet
|
DT |
DS |
DSa |
DSp |
DSp/DSa |
DT/DS |
Total (mm) | 124.14 ± 11.69 | 107.38 ± 13.51 | 66.01 ± 9.15 | 41.36 ± 8.19 | 0.64 ± 0.14 | 1.17 ± 0.17 |
Male (mm) | 119.62 ± 11.60 | 103.01 ± 11.69 | 65.01 ± 8.82 | 38.00 ± 6.61 | 0.59 ± 0.13 | 1.18 ± 0.18 |
Female (mm) | 130.85 ± 8.08 | 113.96 ± 13.48 | 67.53 ± 9.48 | 46.43 ± 7.77 | 0.70 ± 0.14 | 1.16 ± 0.16 |
P Value | 0.0003 | 0.0005 | 0.076 | 0.0002 | 0.0008 | 0.623 |
Fig.3 For any group divided by DSp/DSa, the decile points 1,3 ,and 10 have smaller radii of curvature than the beforeand after points,respectively
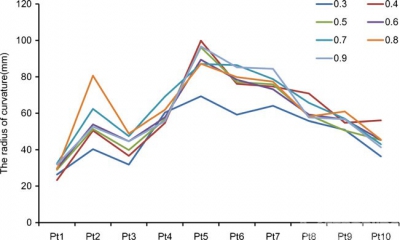
Fig.4 The radius of curvatureat decile point 3 showed an obvious rising trend with therising of DSp/DSa, while the radii of curvature at decile points 1 and 10 had no obvioustrend
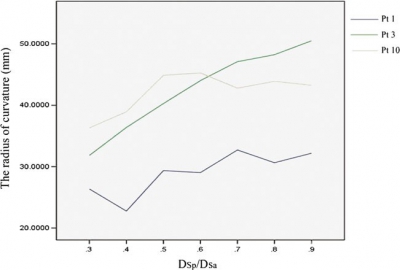
The comparisons between the mean values of the radius of curvature betweentwo adjacent points from decilepoint 1 to 10 showed that the mean value of decilepoint 1 was smaller than point 2, which of point 3 was smaller than point 2 and 4, point 1 smaller than point 9. And there were significant differences between the mean values of the radi- usof curvature at decile points 1 and 2; 2 and 3; 3 and 4; and 9 and 10 (p < 0.05) (Table 6). Hence, for all groups divided by DSp/DSa, the decile points 1, 3, and 10 had smaller radii ofcurvature than the beforeand after points, respectively(Fig.3). The radius of curvature at decile point 3 showed anobvious rising trend with the rising of DSp/DSa. However,theradii of curvature at decilepoints 1 and 1 had no obvious trend (Fig.4).
By dividingthe whole pelvis by DT/DS and repeating thework above, we tried to describe the general situationof the radius of curvature at each decile point for differentDT/DS groups. However, we did not identify any obvious trends.
Discussion
When dealing with peri-anterior column fractures of the acetabulum (including fractures of the anterior wall, anterior column, transverse fractures, T-shaped fractures, fractures of the anterior column or anterior wall associated with a hemi-transverse fracture, and fracturesof both columns) and rotationally unstable pelvicfractures,the superior border of the arcuate line,including its forwardextension,is commonly chosen as the region to place the reconstruction plate. According to the specific fracture type,the reconstruction plate can extend along the pubic tubercle,pubis pectin, iliopubic eminence, arcuate line, or it may approach the sacroiliac joint. This area is considered an ideal Implant location, because it provides clearsurgical exposure, flat bone surface,and relatively thick bone tissue .No anatomical data for the fixation route along the superior borderof the arcuate line is currently available, which is associated with prolonged operation times due to shaping the reconstructionplate during the surgery, breakageof the internal fixatordue to being repeatedly bent, and loss of stageI reduction due to the mismatchin the shape of implantand pelvis. All of these possibilities increase the risk of theoperation and the incidence of complications. The two hypotheses of this study areto beobtain an optimized plateshape of pelvic fixator by digital 3D anatomical measure- ments, which eliminates the prolonged operation time, breakage of the fixator and loss of stage I reduction, and to find the relation betweenDSp/DSa, DT/DS and the shapeof the superior border of the arcuate line, which could be usedas a base on which to estimate the generalshape of the internal fixator by pelvic type.
3D measurement of thefixation route along the superior border of the arcuate line
Since the superior border of the arcuate line isoften used as the position to correct rotationally unstable pelvic fractures and peri-anteriorcolumn acetabular frac- tures, it is of great importance to analyze its 3Dshape. There is no anatomical data for this fixation route currently available.This study built 3D digital models based on large samples of normal adultpelvic high resolution CT images, measured crucial parameters of the fixation route along thesuperior border of the arcu- ate line, discovered criticalanatomical positions for shaping the reconstruction plate, and providedreference for the design of pelvic anatomical internal fixators atthisarea.
According to the results of Table 1, the deviation of thedata was relatively extent.After eliminating the miscalcula-tion, we think it was caused by the manual operation duringthe process of picking the cortical surfacepoints to draw the space curve. As the surface of the pelvis is fluctuating and thevalue of the radius of curvatureis sensitive, the value isaffected by the error of the manual operation.
By combining each decile point’s bending, which can be derived from the radius of curvature, with the actual risingor sinking status of the pelvic surface, it is possible to achieve betterplate-pelvis matchingresults. The total length of the curve (male: 143.47 ± 10.22 mm, female: 151.62±9.67 mm, P < .001) helps in choosing the length of the plate. The bone thickness of each decile point providesreference for the drilling depth and the screw length,which is important in terms of avoiding blood vessel and nerveinjuries. The thinnest bone region of the acetabulum area (male: 15.37 ± 3.08mm, female: 11.89 ± 2.60 mm, P < 0.001) contributes to the accuracy of acetabular screwplacement, preventing the screw from penetratinginto the acetabulum and causing severe complications. The diameters of the pelvic inlet and relatedratio calculations revealthe differ- ences among different pelvic shapesat the fixation route along the superior border of the arcuate line. They also assist inshaping the platesmorequickly and more accurately. Furthermore, the anatomical data achieved in this studyprovides reference for the designof pelvic anatomical inter- nal fixatorsin this area. All samples in this study were healthy adults. Epiphysis for all cases is closed. Therefore, neither age nor changes in the size of the pelvis were considered. Some parameters were statistically significantly ifferent betweenmales and females: DT (male: 119.62 ±11.60 mm, female: 130.85 ± 8.08 mm, P < .001), DS (male:103.01 ± 11.69 mm, female: 113.96 ± 13.48 mm, P < 0.001),DSp (male: 38.00 ± 6.61 mm, female: 46.43 ± 7.77 mm, P <0.001) and DSp/DSa (male: 0.59 ± 0.13 mm, female: 0.70 ±0.14 mm, P < 0.001).
To understand the generaldirection and important turningpoints of the fixation route for different inlet shapes, we divided the entire pelvis into groups by DSp/DSa, and ana- lyzed the radius of curvatureat each decile point for eachgroup. For any group dividedby DSp/DSa, the decile points1,3, and 10 had smaller radii of curvature than the before and after points, respectively.Relating the aforementioned decile points to anatomical positions, we found that for all of thepelvic inlets of different shapes, the curve has a relative- ly greater bendingdegree at the pubic tubercle, iliopubiceminence, and near the sacroiliac joint. For all other loca-tions, it is relatively flat. In clinical practice,the bending of the plate is the vital and complexstep of pelvic and acetab-ular surgery, which is partly the reason why the learning curve of these operations is quite prolonged. According to this study, more bendingshould be conducted at the pubic tubercle, iliopubiceminence and near the sa-croiliac joint during pelvic and acetabular surgery. More comparisons between the key bending points and the adja- centbone surface need to be taken to bend the plate fewertimes. Hence, the time of shaping the reconstructionplate and the breakage ofthe internal fixator could be reducedby accurate and adequate plate bending.
The relation between the shapes of the pelvic inlet and the superior border of thearcuate line:
Unlike other human bones, the pelvic shape appearsmark- edly different between males and females. Even for the female pelvisalone,there are four different shapes,which are termedgynecoid,android,platypelloid and anthropoid. Differences among pelvic shapes are related to the changesof the pelvic inlet shape, in particular,to the ratio of the posterior sagittal diameterto the anterior sagittal diameter (DSp/DSa) and the ratio of the transverse diameter to the sagittal diameter(DT/DS). With the increase of DSp/DSa and DT/DS, the pelvic inlet shape transitionsfrom the heart-shape of the android type to the approximately round, ellipticalshape of the gynecoid and platypelloidtypes. In this study, we analyzed the trends of the radii of curvatureat decile points 1, 3, and 10 with the change ofDSp/DSa. We found that the radius of curvature at decilepoint 3 showed an obvious rising trend with the risingof DSp/DSa .However,the radii of curvature atdecile points 1 and 10 had no obvious trends.It could be interpreted as with the transition of the pelvic inlet shape from android type to gynecoid and platypelloid types, the bone surface at the iliopubic eminence becomes flatter, but there is no obvious trend either at the pubic tubercle or close to the sacroiliacjoint. In addition, we analyzed the trendof the radius of curvature for eleven decilepoints with different DT/DS.This did not reveal any obvious trends, whichmeans it is still not reliable to provide references forthe fixation route along thesuperior border of the arcuate line by the transition of the pelvic inlet shape.In brief,more plate bending should beconducted in gynecoid pelvis than in other types during pelvic and acetabularsurgeries.
Safe paths for screw placement on the anterior column of the acetabulum:
When fixing acetabular fractures through anterior approaches like the ilioinguinal and stoppa approaches, lack of visualiza-tion of the hip joint might lead to improper screw direction or position. The resulting screw penetration into the hipjoint might bring future chondrolysis and osteoarthritis. Previous authors have reported severalmethods to pre- vent this severe complication,including intra-operative radiographs or fluoroscopy and auscultationof the hip with motion in a quiet room, which increase the oper- ation time and trauma. Hence, for accurate screw place-ment, it is imperative to understand the unique 3Dstructure of the anterior column of the acetabulum. Although there are few quantitativeanatomic data on the technique of plate-screw fixation of the anterior column of the acetebulum,some authors have proposedways to avoid this complicationbased on the cross- section of the anterior column. These include: (1) Use of a long screw. Owing to the 6–12 mm thick bone tissue between the surface of the hip joint and the medial quadrilat-eralsurface, ascrew with direction parallel to the quadrilateralsurface will not penetrate into the hip joint. However, due to the restriction of the entry point, this method is suitable forsimple long screw fixation only and not for plate-screw fixa-tion. (2) Use of a short screw. The bone tissuebetween the pelvic brim and the hip joint surface is more than 12.0 mm. Inconsequence, a screw with any angle will not penetrate into the hip joint as long as the length of the screw is shorter than 12. mm. However, the strength of fixation with screws
shorter than 12.0 mm at the anteriorcolumn needs to bevalidated. (3) Insert thescrew at a certain angle. At theentrypoint 1. cm away from the pelvic brim, if the directionof the screw is pointing to the quadrilateral surface and greater than 2°, the screw can be kept away from the hip joint and haveenough length .
This study transected the anterior column of the acetab- ulum perpendicularly to the bone surface at the fixation route along the superiorborder of the arcuate line, andmeasured the minimum thickness of the acetabular area,which is considered to be a safe path for screw placement on the anterior column.The results showed that a screwperpendicular to the bone surface would not penetrate into thehip joint if it were shorter than 14 mm. Compared withthe three aforementioned methods,this study has found a practical solution for plate-screw fixation at this region. However, it stillneeds to be improved upon.
Limitations and shortcomings:
In this study, all subjects were unrelated ethnicHan Chinese recruited from Shanghai First People’s Hospital. It would be interesting to conductindependent studies in other ethnic populations for comparison. In addition, dueto the different medical conditions of each sample, we could not gather thecomplete data of each sample’s height and weight. It would be meaningful to performa follow-up study that expands the analysis, including these parameters.
Conclusion
By digital reconstructionand 3D measurement of a large sample of normal adult pelvicCT scans, this study obtaineda series of parameters describing the shape and bone thick-ness of the fixation route along the superiorborder of the arcuate line to the pubic tubercle, the bone thickness of theacetabular area, and the relative diameters ofthe pelvic inlet.Weanalyzed the differences between male and female,discovered the key bending points of the shape of the internal fixator, discussed the relationship between the pel- vicinlet shape and the internalfixator shape, and provided references for a safe path for screw placement on the anteriorcolumn of the acetabulum.While not addressing soft tissue coverage, surgical exposure, or reduction effects of the frac-tureduring the operation, this 3D measurement study based on the reconstruction of pelvic bone tissue provides a solid reference for clinical applications.



 京公网安备11010502051256号
京公网安备11010502051256号